Konference: 2011 III. česko-slovenská konference paliativní medicíny
Téma: Paliativní medicína v Evropě, v Česku a na Slovensku v roce 2011
Číslo abstraktu: 02
Autoři: Prof. MUDr. Lukas Radbruch
Palliative care has started in Europe in 1967, when Cicely Saunders opened St. Christopher‘s Hospice as the first modern hospice in London. This was built on the tradition of hospices reaching back to medivial times, when hospices were built as guest houses for weary or sick travellers, often attached to monasteries.
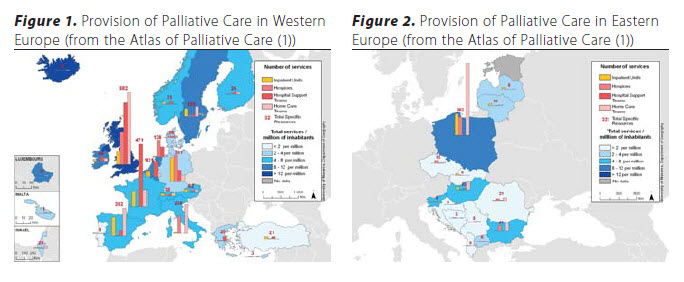
Since then, the modern concept of hospice care and palliative care has increasingly received attention throughout Europe. A growing number or palliative care and hospice services has been established in most European countries, though the development has started later and is going slower in Central and Eastern European countries. Figures 1 and 2 are reproduced from the Atlas of Palliative Care (1) and show the state of service provision in Europe in 2007.
Palliative medicine has also been acknowledged as a specialty of medical training in the United Kingdom and Ireland, and as a subspecialty in the Czech Republic, France, Germany, Poland, Romania and Slovakia. Palliative care is established as an academic field with an increasing number of academic chairs, not only in palliative medicine, but also in policy and organization of care, spiritual care, social care or hospice care.
Palliative care is also recognized on a political level. The Council of Europe has recommended the development of palliative care with its Recommendation 24 in 2003, with an elaborate set of recommendations covering all areas of palliative care from inpatient services to bereavement care (2).
The recent report on palliative care to the parliamentary assembly of the Council of Europe (3) has even described palliative care as a model for innovative health and social policies.
On a national level, national strategies for palliative care are being implemented in several countries, for example in Switzerland or in the United Kingdom (4).
The European Association for Palliative Care (EAPC) was established in 1988, with the aim to promote palliative care in Europe and to act as a focus for all of those who work, or have an interest, in the field of palliative care at the scientific, clinical and social levels. The 12th congress of the EAPC (www.eapcnet.eu) in May 2011 in Lisbon enabled more than 2500 participants from all fields of health care to meet and discuss state of the art treatment and new developments. The mission of EAPC is to bring together many voices to forge a vision of excellence in palliative care that meets the needs of patients and their families. In addition to the biannual congresses and interlaced research congresses the EAPC produces guidance and support, for example with a white book on standards and norms in palliative care (5, 6). With 46 national associations in 27 countries as collective members as well as the individual members EAPC represents well above 50.000 health care professionals and volunteers in palliative and hospice care.
Other developments may be even more important, leading to sustainable social change. In Germany the hospice movement has included more than 80.000 volunteers by now, and volunteer work is not only focused on patient care. In the project „Hospice goes to School“ hospice volunteers organize and run a project week on illness, death and dying in primary schools, with stories, films, playing and handicrafts. The week culminates in a final presentation with the parents, and the discussions the children take back home to their families promote palliative and hospice care even further.
Throughout Europe, examples and advice can be found on most areas of palliative care. As an example from Germany, the conference of federal ministers of building published a howto- do report on the construction of palliative care units, including basic requirements, but also examples from renowned units with floor plans, room size lists and photos. As I am in the process of planning a new palliative care unit, I found this report exceedingly helpful.
However, there is a wide scope of development in the different European countries and regions. A report to the European Parliament produced by Martin Moreno, et al. in 2008 (7) revealed broad discrepancies in the provision of palliative care as well as in the vitality of development between European Union Member States. The statistics suggest profound differences between countries such as UK, Ireland, Sweden and the Netherlands, who were rated highest in these two indicators, and the countries of Greece, Portugal, Slovakia and Estonia. Similarly, the more recent report of the Economist on quality of death (8) ranked the UK highest in the overall score and another 5 European countries among the top 10, but again other European countries such as Portugal, Turkey and Russia scored very low.
These differences are due mostly to the differences in the health care systems in the European countries. Eastern Europe countries lack resources, as the economy is only slowly improving after the end of communist regimes. Legislation on narcotic laws is much more restrictive than in Western European countries (figure 3), and patients will have problems to find a physician with palliative care expertise or to get opioid prescriptions. There are notable exceptions, and the report on palliative care to the European Union in 2009 (3) has identified centers of excellence in Poland, Russia, Hungary and Romania, that set examples for Western Europe as well as for Central or Eastern Europe. Experts in these centers have succeeded in influencing the policy makers to change legislation, make opioids available and even implement palliative care programmes.
The project Access to Opioid Medications in Europe (ATOME), led by the World Health Organization and the universities of Bonn, Lancaster and Utrecht has set up workgroups in 12 Eastern and Southern European target countries in order to improve availability, accessibility and affordability of opioids such as morphine. As a first result of ATOME, the WHO guidelines on accessibility of opioid medications has been revised (9). The guideline includes a checklist that can be used to check the legislation of any country and identify gaps where balance should be ensured.
The provision of palliative care also depends on the underlying disease. Palliative care in Europe is focused primarily on cancer patients, and patients with other diseases such as advanced obstructive pulmonary disease often lack information about the option of palliative care or find it hard to access palliative care services. These disease entities often have more prolonged disease trajectories (10) and accordingly may have other needs than cancer patients.
Problems to access palliative care have also been described for members of other ethnic groups, such as Irish travellers or migrants.These groups may also require specific care. Irish travellers for example may find it rude and intrusive if health care staff discusses prognosis and imminent death. They also might wish to die in hospital rather than at home, as the family might not wish to continue to live in the trailer or home where someone has died (11).
Cultural differences have become most evident in the legalization of euthanasia in some European countries (Netherlands, Belgium and Luxemburg). Differences in the ethical principles and frameworks of palliative care related to the use of euthanasia in these countries have been described.
Cultural difference can also be observed in the ways healthcare provision is organized. An example of this is the role played by volunteers. In some countries volunteers play an integral and key role in supporting hospices and providing care in the home, while in others they are less central. In Germany, volunteers play a substantial role in hospice home care programs. Volunteering is well-organized, and sickness funds provide reimbursement for volunteer coordinators. By contrast, volunteering is a less recognized element in healthcare provision in Spain, where the tasks that volunteers could take on usually are delegated to family members, and the family may consider outside help as an intrusion rather than support (Kathrin Woitha, personal communication).
Language and culture also shape and infuse our attitudes towards death and dying. Words like the French “crever” or German “krepieren” (to die in a terrible way) can be translated in many European languages. However, the distress conveyed by these words cannot be expressed in other languages, for example English, where expressions such as “die”, “perish”, or “kick the bucket” are only weak substitutions (12). Our attitudes to pain and death are so saturated in cultural indicators that they become a part of the stereotype, for example with the English “stiff upper lip”, or the “Mediterranean Syndrome”.
The diversity of needs and delivery may be illustrated with a case example. Angela is 48 years old and has metastatic cancer of the rectum. She cannot obtain adequate symptom relief in spite of treatment with low doses of opioids, but she wants to go home. She has an eight-year-old son, and an abusive husband. She is entitled to respect for her autonomy, but her decision on whether to stay in hospital, to go home, or to enter a hospice, will depend on a number of factors, including: availability of the facilities; community support; the value of autonomy in the individuals and groups concerned; on family tradition; and on the model of decision making which dominates. All this factors will vary from country to country, from region to region, and from family to family.
EAPC has prepared a white paper on standards and norms for hospice and palliative care across Europe based on a consensus procedure with the national associations in the European countries (5, 6). This white paper reports on discrepancies in terminology and differences in the philosophy of palliative care, but also provides standards for structural, procedural and outcome quality of palliative care in different settings. This white paper will be used as a first step towards the development of a European standard providing high quality palliative care to all patients and care givers who need it.

References:
- Centeno C, Clark D, Lynch T, Rocafort J, Flores LA, Greenwood A, Brasch S, Praill D, Giordano A, De Lima L. EAPC Atlas of Palliative Care in Europe. Houston, IAHPC Press; 2007.
- Council of Europe. Recommendation Rec (2003)24 of the Committee of Ministers to member states on the organisation of palliative care 2003. http://www.coe.int/t/dg3/health/ Source/Rec(2003)24_en.pdf (access date: 28.7.2009).
- Parliamentary Assembly of the Council of Europe. Palliative care: a model for innovative health and social policies. Report of the Social, Health and Family Aff airs Committee, 2009. http://assembly.coe.int/Documents/AdoptedText/ ta09/ERES1649.htm (access date: 7.1.2011).
- Department of Health. End of Life Care Strategy. Promoting high quality care for all adults at the end of life, 2008. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/ PublicationsPolicyAndGuidance/DH_086277 (access date: 28.7.2009).
- Radbruch L, Payne S, Bercovitch M, Caraceni A, De Vliege T, Firth P, Hegedus K, Nabal M, Rhebergen A, Smidlin E, Sjögren P, Tishelman C, Wood C, de Conno F. White paper on standards and norms for hospice and palliative care in Europe part 1 – recommendations from the European Association for Palliative Care. European Journal of Palliative Care 2009; 16: 278–89.
- Radbruch L, Payne S, Bercovitch M, Caraceni A, De Vliege T, Firth P, Hegedus K, Nabal M, Rhebergen A, Smidlin E, Sjögren P, Tishelman C, Wood C, de Conno F. White paper on standards and norms for hospice and palliative care in Europe part 2 – recommendations from the European Association for Palliative Care. European Journal of Palliative Care 2010; 17: 22–33.
- Martin Moreno JM, Harris M, Gorgojo L, D Clark, C N, Centeno C. Palliative care in the European Union, 2008. http:// www.europarl.europa.eu/activities/committees/studies/ download.do?fi le=21421.
- Economist Intelligence Unit. The quality of death. Ranking end-of-life care across the world, 2010. www.eiu.com/sponsor/ lienfoundation/qualityofdeath.
- World Health Organisation. Ensuring balance in national policies on controlled substances – Guidance for availability and accessibility of controlled medicines. Geneva, WHO Press; 2011.
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care.. BMJ 2005; 330: 1001–11.
- McQuillan R, Van Doorslaer O. Indigenous ethnic minorities and palliative care: exploring the views of Irish Travellers and palliative care staff . Palliat Med 2007; 21: 635–41.
- Taubert M. Je ne veux pas crever. European Journal of Palliative Care 2007; 14: 78–9.
- Cherny NI, Baselga J, de Conno F, Radbruch L. Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in Europe: a report from the ESMO/EAPC Opioid Policy Initiative. Ann Oncol 2010; 21: 615–626.
Datum přednesení příspěvku: 24. 11. 2011





